By Megan Doyle, MS, OTR/L, FPS, Cert-APHPT
Occupational Therapist, Fellow of Pain Science,
and Certified Applied Prevention Health Promotion Therapist
Sleep Impacts Pain More Than Pain Impacts Sleep
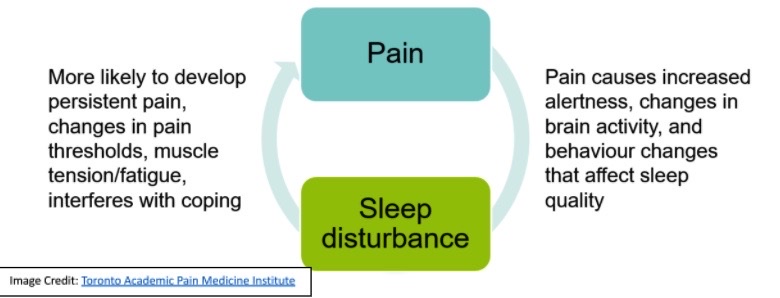
It makes sense that having pain, whether it be in your low back, neck or joints would make it difficult to sleep. But did you know that research has also shown that a poor night of sleep is more likely to lead to the onset of pain? [1,2]
-
- Sleep problems have been shown to both worsen existing chronic pain conditions, but also increase the risk of onset of chronic pain in prior pain-free individuals. [1,3]
-
- In one study [1], healthy subjects reported spontaneous bodily pain after 2 nights of partial (4 hours) sleep deprivation, and this effect increased as the number of nights of partial sleep deprivation increased.
-
- Another study [4] found specifically in working individuals, sleep problems predicted the onset of both low back pain, but also emotional distress and work burnout, demonstrating the psychological effects in combination with pain onset from poor sleep.
-
- Poor sleep has even been found to be a greater factor in the prevention of pain than routine physical activity, as a study [5] focused on the health of adults over 50 noted that “the beneficial association of physical activity on reduced likelihood of later pain was only observed in persons who endorsed low levels of sleep disturbance” (pg. 1).
Your Brain and Body on Lack of Sleep (and Why It’s Such a Pain)
Yikes! So, now that I’ve got your attention, perhaps you’d like to know a little bit more about the mechanisms behind the relationship between sleep disruption and pain onset. This will allow for you to understand not only why it occurs, but more importantly, how you can reduce your risk (more on that later). The following information is referenced from Pain Psychologist Kern A. Olson, PhD’s article entitled “Pain and Sleep: Understanding the interrelationship” [3].
-
- Sleep is critical for maintaining homeostasis (equilibrium) in our bodies, and we need routine, quality sleep to survive and cope with the demands of everyday life.
-
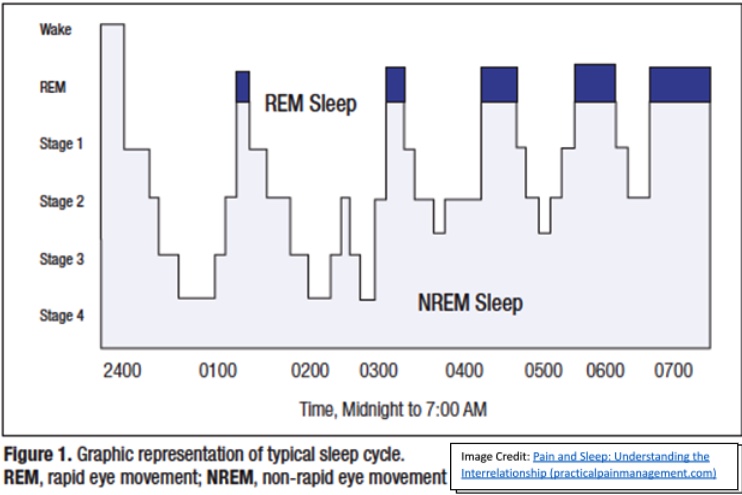
- The sleep cycle is divided into two main areas: “non-REM sleep” and “REM sleep”, where “non-REM sleep” is further divided into “light” and “deep” sleep components.
-
- Non-REM sleep is important for both brain and body restoration, whereas REM sleep is when we dream and has been found to be the part of the sleep cycle that is crucial for maintaining our mental wellbeing.
-
- The average adult spends about 75% to 80% of their sleep cycle in non-REM sleep and about 20% to 25% in REM sleep
-
- Specific brain regions play a critical role in sleep regulation, as they do in pain regulation. For instance, research has shown that damage to a brain area called the anterior hypothalamus caused severe insomnia.
-
- The hypothalamus is involved in controlling both waking and sleeping states (including generating non-REM sleep) as well as in the control of pain.
-
- Another brain region, called the basal forebrain, is also involved in generation of non-REM sleep.
-
- It should be noted that both the hypothalamus and the basal forebrain contain the neurons active gamma aminobutyric acid (GABA), which play a pivotal role in (you guessed it) the control of pain and sleep.
-
- In addition, REM sleep is controlled primarily by the brain stem, which also overlaps with the neural control of pain.
-
- Another key hormone in the regulation of both sleep and pain? Dopamine, which also helps to regulate mood state, and dysregulation of the dopamine system may also lead to persistent insomnia or sleepiness.
In short, there is cross over between the areas of the brain that help to regulate pain processing, and are involved in sleep, leading to an important need for quality sleep to decrease the risk of pain onset and reduce pain when it strikes.
References:
- Finan, Patrick H et al. “The association of sleep and pain: an update and a path forward.” The journal of pain vol. 14,12 (2013): 1539-52. doi:10.1016/j.jpain.2013.08.007 Retrieved 05/23/21 from: nihms521705.pdf
- Lewandowski Holley, Amy et al. “Temporal daily associations among sleep and pain in treatment-seeking youth with acute musculoskeletal pain.” Journal of behavioral medicine vol. 40,4 (2017): 675-681. doi:10.1007/s10865-017-9847-x Retrieved 05/23/21 from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5912262/pdf/nihms959024.pdf
- Olson, Kern A. “Pain and sleep: Understanding the interrelationship. Practical pain management vol. 14,9 (2015). Retrieved 05/23/21 from: Pain and Sleep: Understanding the Interrelationship (practicalpainmanagement.com)
- Elfering, Achim et al. “Impaired sleep predicts onset of low back pain and burnout symptoms: evidence from a three-wave study.” Psychology, health & medicine vol. 23,10 (2018): 1196-1210. doi:10.1080/13548506.2018.1479038 Retrieved 05/23/21 from: Microsoft Word – PHM2018 final for use.doc (researchgate.net)
- Whibley, Daniel et al. “Sleep disturbance as a moderator of the association between physical activity and later pain onset among American adults aged 50 and over: evidence from the Health and Retirement Study.” BMJ open vol. 10,6 e036219. 7 Jun. 2020, doi:10.1136/bmjopen-2019-036219 Retrieved 05/23/21 from: e036219.full.pdf (bmj.com)
- Scholl, Juliann. “How to sleep better when stressed.” Sleep.org. 26 Mar. 2021. Retrieved 05/23/21 from: Tips to Sleep Better When Stressed | Sleep.org



